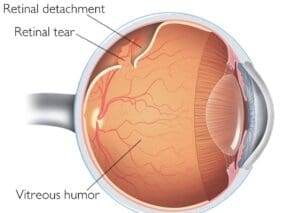
Vitrectomy is often part of another eye treatment e.g. when surgical repair is required for the retina when is detached. Your consultant ophthalmologist may recommend a vitrectomy if you have one of these conditions:
- Diabetic retinopathy, with bleeding or scar tissue affecting the retina or vitreous gel
- most forms of retinal detachment (when the retina lifts away from the back of the eye)
- Macular hole (a hole or tear in the macula)
- Macular pucker (a membrane which wrinkles or creases in the macula)
- Infection in the eye called endophthalmitis
- Severe eye injury
- Certain problems from cataract surgery