Floaters in eyes appear as small dark shapes, spots, or strands drifting across your vision, while flashes are brief streaks of light, often resembling lightning or flickering. Flashers and floaters are more noticeable when looking at bright backgrounds, such as the sky or a white wall.
Flashes and Floaters
Flashes and floaters in eyes are common visual disturbances that many people experience at some point. While they are often harmless, they can sometimes indicate an underlying eye condition that requires medical attention.

What are Flashes and Floaters?
Symptoms of Flashes and Floaters
Symptoms of flashes and floaters in eyes to watch out for:
- Small spots, strings, or cobweb-like shapes drifting in your vision
- Flashes of light, particularly in peripheral vision
- A sudden increase in floaters or flashes
- Shadows or dark areas in vision (may indicate a retinal tear or detachment)
If you notice a sudden onset of floaters and flashes in eyes, especially with a loss of peripheral vision, seek immediate medical attention, as this could be a sign of a retinal tear or detachment.
Causes of Flashes and Floaters
Flashes and floaters in eyes are usually caused by changes in the vitreous – the gel-like substance inside the eye. As we age, the vitreous naturally shrinks and becomes more liquid, leading to tiny fibres clumping together and casting shadows on the retina.
Common causes of flashes and floaters in eyes:
- Natural ageing of the vitreous (most common cause)
- Posterior Vitreous Detachment (PVD)
- Retinal tears or detachment (urgent attention required)
- Eye injuries or trauma
- Inflammation inside the eye (uveitis)
- Bleeding within the eye
Types of Floaters in Eyes
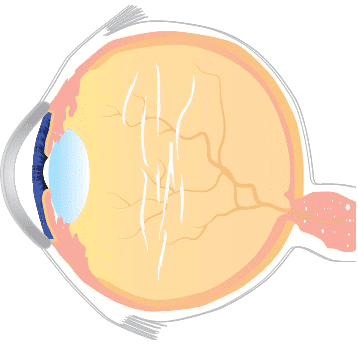
Fibrous Strand
Most common in young people, this thin, dense floater can appear as multiple dots and/or string-like cobwebs and is a result of clumping of the collagen fibers of the vitreous. Depending on size, and where it is located, it may be treatable with vitreolysis.
Diffuse Floater
This cloud-like floater is caused by the natural aging process. Whilst this type of floater can sometimes be treated with vitreolysis, it often requires more overall treatment in order to obtain satisfactory results.
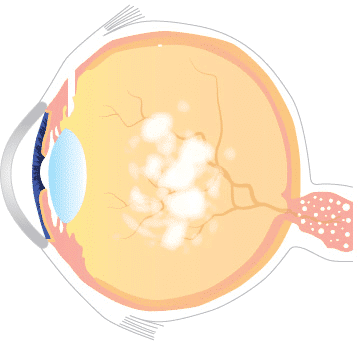
Weiss Ring Floater
The ring-shaped Weiss Ring floater is a large, fibrous floater that is usually located safely away from the crystalline lens and the retina. Because of this, it can be treated safely and effectively with vitreolysis.
Available Treatments
Most cases of floaters and flashes in eyes do not require treatment, but if they become particularly bothersome or indicate a retinal issue, medical intervention may be needed.
Treatment Options:
- Observation – In many cases, floaters fade or become less noticeable over time.
- Laser Vitreolysis – A laser treatment that breaks up large floaters to improve vision clarity.
- Vitrectomy – A surgical procedure that removes the vitreous gel, eliminating floaters but carrying some risks.
- Retinal Treatment – If flashes or floaters in eyes are caused by a retinal tear, laser or cryotherapy may be necessary to prevent detachment.


Price of Treatment
The cost of treatment for flashes and floaters in eyes varies depending on the procedure and individual case. A consultation is required to assess suitability and recommend the best option.
- Initial Consultation: £445
- Treatment From £1,779 per eye (up to 3 treatments)
For a personalised assessment, please book a consultation with our expert team.
Additional Information
Most floaters and flashes in eyes are harmless and part of the natural ageing process. However, a sudden increase in floaters, flashes, or loss of vision could indicate a retinal tear or detachment, which requires urgent medical attention.
Floaters in eyes can be a symptom of posterior vitreous detachment. This is a common condition that occurs in about three-quarters of people over 65 years of age. PVD can occur as the result of changes to the vitreous humour as the eye gets older.
As we get older the central part of the vitreous humour becomes more liquid and the outer part, known as the cortex, starts to shrink away from the retina. Floaters are created as a result of the collagen clumping together.
Flashing lights can also be another symptom of PVD. Flashing lights may occur when the outer vitreous humour pulls on the light-sensitive tissue of the retina. The pulling on the retina causes brain to interpret it as a light signal.
Floaters in eyes may be a sign of retinal detachment (when the retina separates from the wall at the back of the eye). If you have retinal detachment, you will usually have:
- a large number of floaters
- flashing lights
- loss of vision
There are several types of surgery to repair a detached retina. The type of procedure your Consultant Ophthalmic Surgeon performs will depend on the severity of retinal detachment.
If you think that you may have retinal detachment, seek urgent medical attention from your GP or optometrist (optician). If you are patient of Centre for Sight already please call 0808 291 5658.
Over time, floaters often settle or become less noticeable. If they significantly interfere with vision, treatments like laser vitreolysis or vitrectomy may be considered.
While they cannot always be prevented, maintaining good eye health, managing conditions like diabetes, and wearing protective eyewear to prevent eye injuries can help reduce risk of floaters in eyes.
Seek medical advice if you experience:
- A sudden increase in flashes or floaters in eyes
- Loss of peripheral vision
- A shadow or curtain effect in your vision
- Eye pain or redness alongside floaters
If you’re experiencing any concerning symptoms, book an appointment with our specialists today. Early detection and treatment can help protect your vision.
Author Information
Authored by Sheraz Daya MD FACP FACS FRCS(Ed) FRCOphth, Consultant Ophthalmic Surgeon & Medical Director, June 2019.
Next review due August 2025.