Adaptation (Neuro-adaptation)
When one eye is treated at a time, patients often report the following day that their vision in the treated eye is not quite as good as expected. This is often the case in those who were previously farsighted and can find that distance vision is blurred. This happens because the eye muscles which are trying to focus in the untreated eye, result in the implant being pushed forward making the patient short-sighted. For those previously shortsighted, distance vision is reported as very good, however near is initially a struggle and with adaptation improves. The brain eventually picks up the information that it needs and vision improves. With trifocal lenses, we emphasise preoperatively that it is only when BOTH eyes are treated that patients get the benefit from the lenses with no comparative reference points. The eyes see similarly and vision improves rapidly each day.
Visual side effects
Initially halos around headlights interfere with the ability to drive comfortably affects 10% of patients, but improves in all patients with time. With adaptation, the brain is able to suppress unwanted information and patients report noticing a reduction in the size of the halos over the next 6 to 12 weeks, eventually disappearing or being just a nuisance. A few patients take longer to adapt (12 to 18 months). In the worst case scenario the implant can be replaced at a cost with a monofocal lens, which will have the consequence of reducing the depth of focus and result in the need for glasses.
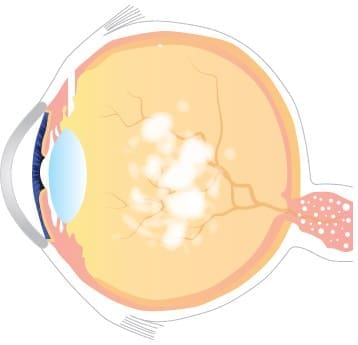
We check for dry eye before surgery and this is treated if found to be significant. Those with marked tear surface abnormalities are not suitable for multifocal lenses. The abnormal surface can affect the performance of the lenses and cause fluctuation in vision. This condition can be treated in advance and once better, patients can be considered for multifocal lenses. Dry eye after lens replacement surgery can occur as a result of a) no longer wearing glasses or contact lenses and being exposed to the elements or more commonly b) toxicity from the eye drops which are at a high concentration in order to penetrate and enter the eye. Preservatives in drops are also a contributory factor. Dry eye symptoms and effects do improve a few weeks after the course of eye drops has been completed.
Reading and intermediate vision
Trifocal lenses distribute light energy to three points of focus. The majority (60% or more is for distance and the remainder for intermediate and near. Also, some trifocals have more energy concentrated near the centre of the lens, as pupils typically constrict when one reads. However, in dim light, the pupils can dilate and thus affect reading performance, so reading menus in a dimly lit restaurant might be problematic. Using a light to illuminate the object should help. The ability to see at intermediate (computer monitors) can in some patients take time (6 to 12 weeks) and again this is to do with adaptation. The brain adapts and uses the information that is being transmitted from the retina.